Providing quality care is stressful. Software shouldn’t be.
Get comfortable. We empower human service agencies and caregivers with person-centered modern tech and human support to deliver more care, more easily and efficiently – all while getting paid faster, with confidence.
We are stronger, together.
We see you. We’re here to help.
Late nights, early mornings, skipped lunches, working while sick – all trying to keep up with billing, compliance, payroll and managing employees. There is a better way.
That’s why Pavillio is here to help you and your team – and get started and see the impact of Pavillio in 30 days.
In fact, we have a new resource to help. Start your journey by downloading our guide “Top 7 Questions To Ask In Your HCBS Software Search.”
Programs we serve
Complete compliance. Complete care.
Home & Community
Learn more
Residential & Group Homes
Learn more
Day & Vocational
Learn More
State & Local Government
Learn More
Financial Management Services (FMS)
Learn More
Housing Stabilization
Learn More
Who Pavillio Helps
We support the unique needs across the complete care community
Home & Community-Based Services
(HCBS) Agency Providers
Electronic Visit Verification (EVV) Compliance
One-click billing – 99% payment on first submission
Digital documentation with custom forms
Employee payroll
Automated eligibility
Caregivers
Advanced mobile app designed for caregivers
App supports 10 different languages
Manage hours worked and overtime
Real-time communication with agency
Track non-billable time
Individuals & Families
Mobile app to review and approve visits
Portal to review care history
Easy access to service auth and hours available
Single login for multiple roles
State & Local Government
Streamline MCO payments
Out-of-the box integration
Resident mobile app for government services
Data portability between government agencies

Caregivers at the Core
Real talk. Caregivers make it all possible. Clilents wouldn’t get the same outcomes without them. Because of them, your clients and the I/DD community can thrive, not just survive.
See Pavillio in Action

Person-focused design
See one-click billing in action
Watch the short video
Pavillio is the backbone to helping you manage and deliver care
Your caregivers and human services teams are critical to improving outcomes. That’s why you need a partner with technical and industry know-how to help you. Another bonus? Your team will love us.
Electronic Health Records
(EHR)
The order and clarity you need for complete documentation
Consumer-Driven Self Service
Bring the team together and empower individuals with I/DD to self direct their services
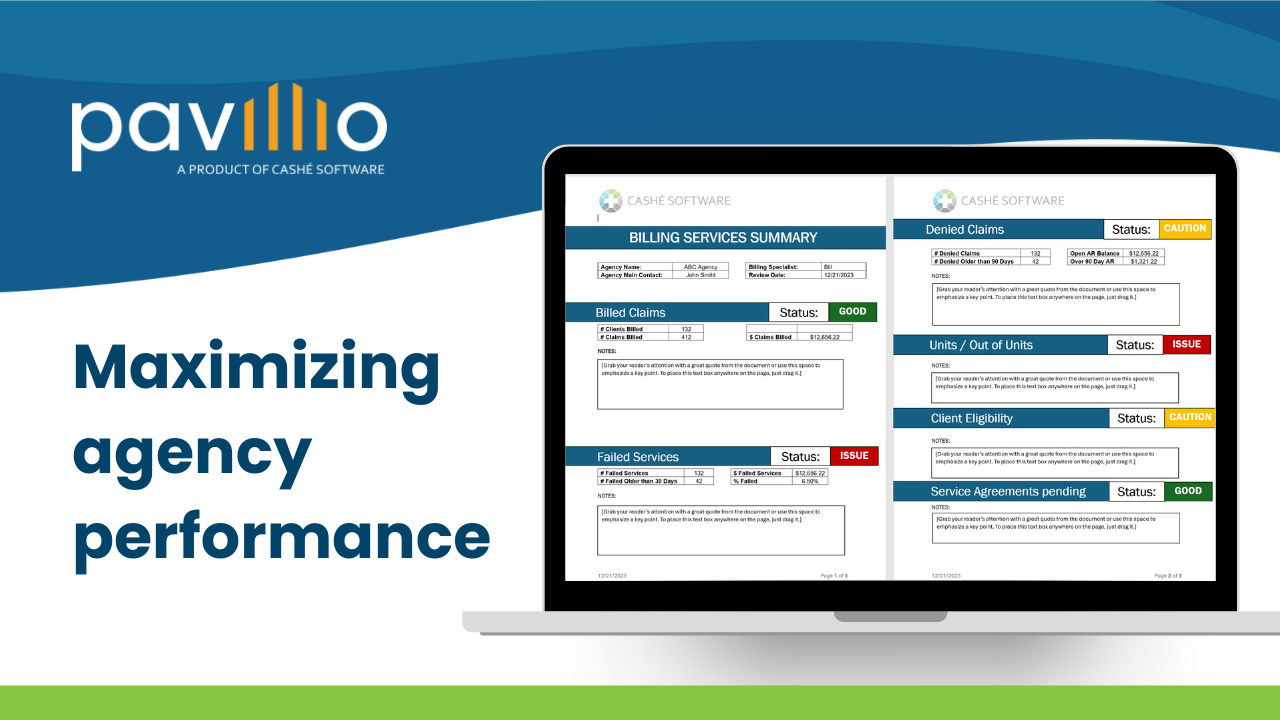
Billing & Revenue Cycle Managment
Track and optimize claim management to more confidently forecast financial performance and post claims revenue faster.
What our customers have to say about Pavillio
Trusted by more than 70,000 caregivers

Lola Aune, Director of HR
Udac, LLC

Aandrea LaFavor, Project Manager Midwest Independent Living Services

Colette Sanyl, COO/Programs Director CJS Community Services, Inc.
home care & community services agencies choose us
%
claims paid when submitted the first time
$2B
Medicaid payment processed
%
of manual tasks now automated
caregivers trust and use us
Pavillio Customer Support
4.7 out of 5 stars
The Pavillio promise: purpose-driven, person-focused
We’re a human services team at heart with a passion for using technology for good. We help people with disabilities lead meaningful lives.
This is why Pavillio empowers people to connect and collaborate with each other across the care ecosystem to help our communities thrive.
Our guiding principles are to:
Set a new standard

Answers to your most
frequently asked questions
How much does Pavillio cost?
We offer affordable, flexible pricing plans that scale with your agency’s growth. Contact us to learn more.
What programs and services do you support?
See how Pavillio can work for you.
Latest Resources

Delivering maximum impact in 2024 to help you deliver more care, more efficiently
Learn how
How to improve home care billing and payments
Learn how

How Garcia Services, LLC cut its weekly administrative hours by 20%
Learn how
